Multiple states have not been able to implement many of the healthcare policies, as funds are not released in a timely manner by the centre, which results in poor implementation and public healthcare gaps
Then came the Covid-19 pandemic, which not only exposed healthcare deficiencies at every level, but also laid bare the stagnant public healthcare spending and poor implementation of policies by states
Has India got its healthcare policies and priorities wrong, and what would it take to build the infrastructure parallelly with the government with increased participation from startups?
Dissecting India’s Healthtech
India's healthtech startups were growing rapidly even before the pandemic, but Covid-19 has ushered in a new age. This series dives into the trends, startups business models emerging in the wake of Covid-19.
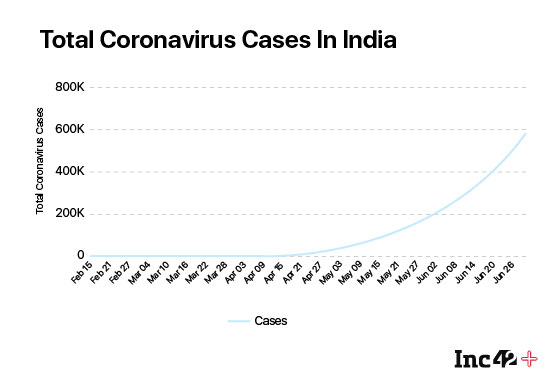
The Covid-19 pandemic has badly exposed the healthcare system of India at almost every level. While the prolonged lockdown had initially kept the rate of active cases in check, the recent growth rate has been exponential and India has overtaken Russia to have the third-highest number of confirmed Covid-19 cases, behind the US and Brazil.
And, there is a long list of reasons for India having badly failed in flattening the curve, from the low rate of testing to the poorly enforced lockdown rules in certain parts of the country.
“In India, if you see, people don’t take their health as seriously as they do other things in their lives. People plan for the house, their marriages… they plan for everything, even for the honeymoon, but they hardly plan for health, which is quite ironic,” explains Dr. Amit Jotwani, cofounder and CMO of virtual cancer care platform Onco.
Despite the harsh truth that our health is bound to deteriorate over time as we age, Indians don’t plan much for it, says Jotwani. Since it’s not on our priority list, the governments — states as well as the centre — too have not prioritised healthcare infrastructure, he claimed.
Dr Jotwani is not alone in claiming this and many have backed this notion that India only takes healthcare seriously when the emergency has already entered the home. Sadly, this time it was a pandemic that served as a wake-up call and the government hurriedly approved telemedicine guidelines on the first day of the nationwide lockdown.
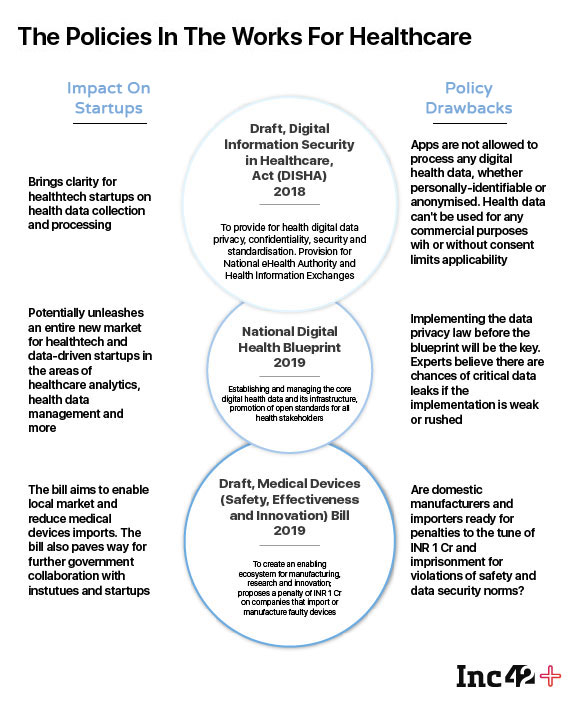
The quick action around the telemedicine policy proves that indeed the government can do things if pushed into a corner. Despite the policy though, the efficacy of telemedicine and chances of it attracting big investments are in question as supporting policies such as the epharmacy policy, the Digital lnformation Security in Healthcare Act (DISHA) and the Personal Data Protection Bill (PDP Bill) among others, that are essential to the healthtech infrastructure have been pending approval for many years.
Right from providing Covid-19 testing services at home to building a host of apps for it and robots for providing essential services, startups in a short span of time have helped India weaponise it against the pandemic. However, given the scale of requirement, the contribution and participation of startups in healthcare have been very limited, Thanks to the lack of policies and in particular, startup-friendly policies.
In western democratic countries such as the US, governments are made and broken based on their healthcare policies. Barring the allocations set in the annual budgets, the current Narendra Modi-led government has taken a slew of measures and has already introduced a number of laws in the last six years.
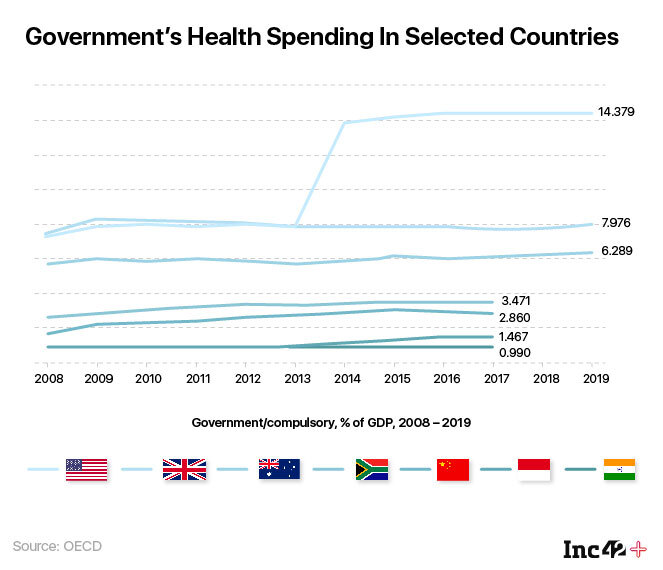
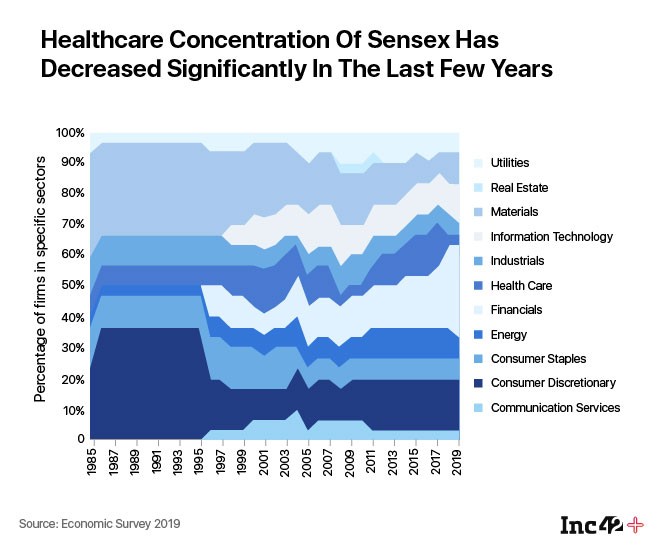
In India, however, healthcare has never been the core part of the government’s budget as well as agenda. Be it the low annual budget expenditure on healthcare — which at just over 1% of India’s GDP is one of the lowest in the world — or the disparate healthcare policies rolled out by many governments over the years — India has never been able to catch up in the global healthtech race. Is the infighting between policymakers at the central and state level to blame, or is the rot deeper?
Have we got our healthcare policies and priorities wrong? What would it take to build a parallel infrastructure with increased participation from startups and investors?
Stagnancy Breeds Rot In Healthcare
“Spending around 1% of the GDP on healthcare, India is in the bottom rung of the ladder across the world. The developed countries, especially the US, spend around 10% of GDP on healthcare. Over the next few years, India needs an investment of at least $60-70 Bn in order to reach the average levels of healthcare infrastructure, leave aside the best.”- Rahul Agarwal, Quadria Capital
Since 1983, when India announced and framed its first-ever national health policy, ‘Health For All’ has been a key objective, an objective which has remained unfulfilled till date. One of the key reasons behind this has been the low government spending on healthcare. If National Health Policy 2002 aimed to spend 2% of the GDP on healthcare by 2010, the updated policy in 2017 aims to spend 2.5% by 2025. The reality, however, is that the public health investment in the country was 1.3% in 1990 and is still the same.
This story is quite opposite to the rest of the world’s. According to the World Bank, between 2000 and 2017, overall health spending dramatically increased in the group of 42 countries that experienced fast economic growth. On an average, real health spending per capita grew 2.2x and increased by 0.6 percentage points as a share of GDP. For most, the growth of health spending was faster than that of GDP, unlike India.
The stagnant budget expenditure can’t simply help achieve the ‘Health For all’ objective. Clarifying it further, Dr Ruchir Mehra said, “The actual budget expenditure is usually less than that of budget estimates.” Mehra is the cofounder of Remedo, a platform for doctor practice management, patient communication and patient engagement.
In contrast to the proposed budget estimates of 1.3% of the GDP, India only spent 0.95% of its GDP in 2017-18, consolidated among state and central government spending. This is against a target of 2.5% that the National Policy on Health 2017 aspired for. The low expenditure in this critical sector is much below international norms, observed 15th Finance Commission in its annual report.
India’s total healthcare spending which includes public, as well as out-of-pocket too, has reduced significantly from 5.2% of GDP in 1990 to 3.6% of GDP in 2018 now. This is significantly lower than the aggregate of OECD countries which was 8.8% of GDP in 2018.
Terming the government’s efforts on the policy front as ‘encouraging’ Meena Ganesh, CEO and MD of home healthcare services provider Portea Medical pointed out that there are several uncovered areas that need to be addressed in order to create a robust and modern healthcare system. There are areas of overlap which result in the lack of clarity about the scope of different schemes at times. Further, there is not yet adequate involvement of the home healthcare or healthcare innovation providers overall.
“The need of the hour is to clearly outline the coverage under each of these schemes and expand the scope wherever needed to make them more effective. Subjects related to insurance coverage for non-institutional healthcare, digital healthcare and diagnostic devices and guidelines for home healthcare need deeper focus,” said Portea’s Meena Ganesh.
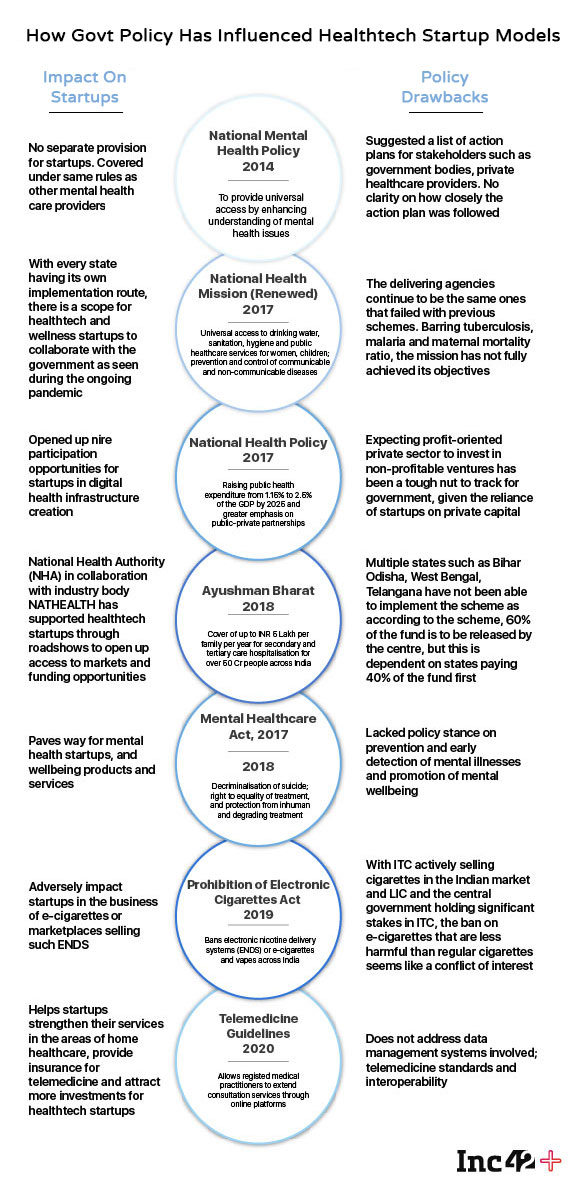
Startups have termed these policies reactionary, and partly anti-industry in the case of products such as e-cigarettes. For instance, telemedicine guidelines, which were released only on March 25, 2020, the same day when the Covid-19 pandemic lockdowns began, needs some refinement as well and ignores some obvious concerns.
The guidelines would help patients and RMPs (registered medical practitioners) to get connected via intermediaries. The Guidelines while mandates patient’s consent for his/her data sharing, and has put the onus on the doctors to maintain the patients’ privacy, it doesn’t delve into the nitty-gritty of data privacy issues.
The government intends to enact the draft Digital lnformation Security in Healthcare Act (DISHA) to provide for electronic health data privacy, confidentiality security and standardization and provide for the establishment of National eHealth Authority and Health lnformation Exchanges. However, the draft that was released over two years back, has not been enacted yet and hence downgrades the real potential of telemedicine in India.
Extending insurance to telemedicine has been a breakthrough and essential development. Prashant Tandon cofounder and CEO of online pharmacy and healthcare platform 1mg said, “The insurance which earlier hadn’t recognised telemedicine has acknowledged this recently. This will bring more investments and traction to telemedicine.”
“The Government of India has acknowledged the need and initiated the formulation of rules related to home healthcare. By bringing these services and innovations under the ambit of health insurance will be further instrumental in the wider adoption of such practices and improvement in the overall healthcare scenario in the country.” — Portea’s Meena Ganesh
Healthcare Being A Part Of List II Make It More Contentious, Less Collaborative
The Covid-19 cases continue to increase on a daily basis. The most affected states Delhi and Maharashtra, in spite of having the best of Indian healthcare systems have been suffering a huge crunch of beds, ventilators in the state. As a result, the Delhi government recently announced a complete reservation of state-backed hospitals as well as private hospitals for the local residents, creating a furore among the residents.
While the decision was later turned down by the Centre, it sparked a fresh debate on whether “public health and sanitation: hospitals and dispensaries” should be categorised in List II (State subject) or List III (Concurrent subject). Something that was discussed in detail during the Constituent Assembly debates too.
A contrarian by choice in the Constituent Assembly debates, HV Kamath had stated on September 2, 1949, “During the British Regime it (healthcare) was especially so, very sadly neglected and not much provided for : as a result of which the health of the nation has fallen to C-3 standards, it is the object of our government today to raise the health of the nation from C-3 to A-I standard. If this were the aim of our Government we could not do better than make public health a Concurrent subject. It must be accorded top priority if the nation is to rise to its full stature.”
Agreeing to the amendment proposal that healthcare should be moved to concurrent list, another member T.T. Krishnamachari, who went on to become the finance minister of India in 1958, seconded the amendment, “I might mention that in regard to public health legislation, the Health Ministry wanted to take it over, and make it a Concurrent subject. As has been explained on a previous occasion.”
Another member Dr. PS Deshmukh had then responded, “The Health Ministry, Sir, is not the last word here.”
Well, 1949 or now, things haven’t changed much. The Delhi government’s banter with the centre is happening at the cost of many lives in the times of Covid-19. The private hospitals on the other end are accused of pickpocketing, charging insane amounts from patients.
On the worsening public healthcare issues in India, Remedo’s Dr Mehra said, “There are so many variables that it becomes a complete mess in terms of accountability.”
Mehra’s statement could also be understood by the fact that even though healthcare at large is a state affair, Article 249 of the Constitution has empowered the centre (Parliament) to make laws on the state list matters citing national interest.
Public health is a state matter; however, public interest has been in the union list. Hospitals fall under state list, the medical education is however guided and controlled by the Centre. In such a situation a medical college which is essentially a hospital thus has to be accountable to both central as well as state machinery. This also opens room for dual corruption and mismanagement.
Is there anything wrong in India’s approach to handling healthcare systems in the country?. “Undoubtedly yes,” said a NITI Aayog officer on the condition of anonymity.
“Let’s take Covid-19 preparations for instance. While the Centre had rightly imposed a nationwide lockdown in the public interest, the lack of coordination among states and preparation at the state level has backfired at many levels. This could have been avoided if healthcare were in the concurrent list,” the Niti Aayog official added.
Earlier this year, a High-Level Group formed by the 15th Financial Commission recommended that right to health be declared as the fundamental right by 2022 and that ‘Public health and sanitation: hospitals and dispensaries’ be moved from List II to List III.
And, there are reasons behind the recommendations. Out of 36 states and union territories, over 24 states and UTs are doing fairly poorly in terms of their state incomes. States like Bihar, Odisha, Uttar Pradesh and West Bengal have huge population but lowest income among the states and hence have been unable to cater to demands.
According to T.S. Vijayan, the chairman of Insurance Regulatory and Development Authority of India (IRDAI), 62% of the total medical cost of India is ‘out of pocket’ expenses i.e., the people paid for those expenses out of their own pockets, which is quite high when compared to the US in 13.4% and the UK at 10%.
This also runs against the grain of India’s social fabric where over 80% of Indians don’t have any form of health insurance. According to India’s National Survey Office (NSO) of the Ministry of Statistics and Programme Implementation, only 14.1% in rural areas and 19.1% in urban areas had any form of health coverage.
While Ayushman Bharat now intends to cover the health expenditure of 53 Cr Indians, in its absence 80% of Indians with no insurance simply can’t afford to get treated in private hospitals.
The government has not been able to crack the execution part of the policies. That’s been the general notion of stakeholders, Inc42 observed. Despite states having badly failed in executing public-private partnership (PPP) projects with startups and other healthtech companies, the NITI Aayog has instead of finding the loopholes behind the failure is mounting on the same school of thought. In its guidelines for the PPP projects in healthcare, the World Bank has been appointed to provide technical assistance for development of the PPP model and a draft model concession agreement for engaging with the private sector.
Karnataka, the state that has been at the forefront of executing PPP projects in the state, had scrapped its PPP project Arogya Bandhu long back in 2016. In other states too, the majority of PPP pilot projects didn’t meet the desired objective and were shut down.
Dr Sylvia Karpagam, public health researcher had then pointed this out that why to involve the World Bank if the government can’t hold the World Bank accountable. Dr Karpagam said, “The World Bank has been at the forefront of pushing for structural adjustment programmes, user fees, PPPs, and generally opening up the market for the social sector. When some of these models promoted by the World Bank have failed and caused damage to comprehensive access to healthcare and derailed public systems, has this body been held to account? Is there even a system in place to hold the World bank to account for the disastrous policies that it has introduced in different countries?”
PPP projects have not only failed in primary healthcare but tertiary as well. For instance, the Rajiv Gandhi Super Speciality Hospital that was rolled out by the Karnataka government in Raichur in tie-up with Apollo Hospitals was later found to be in poor state and the Apollo’s contract was terminated in May 2012.
Not only the PPP projects but the public as well as private healthcare have not been able to provide a successful model. Private players that are there for profits be it pharma or healthcare have their own fair share of criticism of government policies as the government does control in terms of prices, takes much longer time in the approval process.
Given the significantly lower India’s per capita income, the government too can’t let private players alone dictate the pricing.
The infighting in various forms among various players thus has continued. Schemes and policies such as Ayushman Bharat are in tatters because of this policy muddle.
Started in 2013, the National Rural and Urban Health Missions have met with limited success. India’s primary healthcare has only collapsed over the years. Pointing this out, Onco’s Dr. Jotwani said that primary healthcare has been totally missing. India has been reactionary in many ways. Whatever government has done is only related to new medical colleges, or some district hospitals, but no one in the ecosystem, especially the administrative side of things, had any idea how to deal with a pandemic. “And we have been lucky. I would say if we had seen, if we had that virulent strain or our immunity was not so strong, or if you were seeing those kinds of numbers as in the US, you can’t even imagine what the fatalities would be like. That was the most worrying factor in the medical fraternity,” the Onco founder added.
The Fix For India’s Healthcare
Had there been an enabling healthcare policy for startups, people in self-quarantine could have been easily treated via telemedicine and with epharmacy services and diagnostics startups bridging the other essential gaps! This would have reduced a great burden in terms of beds, and most importantly the state of unrest, at least in urban parts of the country.
1mg’s Tandon argued, “While we have done better than most of the countries the challenge has been in scaling up the available solutions. For instance, back in 2012, China had started the concept of internet hospitals. So, when Covid-19 happened China had already a strong home healthcare system in place which helped immensely in lockdown and self-quarantine.”
Public healthcare is in very bad shape. Even politicians won’t go to public hospitals and private hospitals would only invest in areas where they can get a reasonable revenue, argued Dr Jotwani. “That’s why primary healthcare is not a piece of cake because no one knows primary healthcare needs more of an investment than returns. But it builds the overall healthcare of the population. If you have a very sound primary healthcare in general, you would see a better life expectancy.”
In order to address the primary healthcare deficiencies, the centre has now approved and released telemedicine guidelines which would help patients get instant consultation via various platforms offering services through registered medical practitioners.
This is just one step. Portea’s Ganesh said that since the pandemic has spread at a very rapid pace, the need today is to augment the existing healthcare infrastructure with available and scalable alternatives in areas of healthcare innovation, doorstep delivery of professional healthcare, telemedicine and diagnostic services. “These services act as force multipliers and enable doctors engaged in conventional clinical/hospital services to provide consultations to patients remotely,” she added.
Telemedicine in India has a very limited appeal at the moment. In India, people have age-old tendencies to physically visit a doctor. This will take at least the next 5-10 years to change. eExpedise Group, a platform which enabled foreigners to consult Indian doctors, had recently introduced telemedicine services on its platform as part of a pilot project. The project was run in Bihar and a couple of other states, however, just nine patients used the platform for telemedicine services.
CEO Amit Sharma told Inc42, “Telemedicine has its limitations, particularly in India. This seems to be quite popular in metro cities of India, however, in other areas, there are behavioural issues which will take its own time to change. Based on our own experience in this regard, I would say, despite telemedicine usually offering a cost-effective solution, people prefer to go to the doctor and show physically. And, it will take a generation to change the behaviour, if we start today.
Besides the behavioural issues, there is a host of supporting policies as mentioned earlier that need to be implemented before telemedicine gets the working for every stakeholder. For instance, the epharma and DISHA as pointed out earlier has still not been enacted.
Quadria Capital’s Agarwal believes the government has been listening to startup and private sector feedback. While most of the policies have been there and the major issues have been with their implementation part, and the lack of pharma policy has also been a major hurdle. “We have looked at many pharmacies as potential investments and there is always an element of doubt around the regulatory framework for those.”
It’s ironic that pharma stores can sell any medicine without seeing a prescription. No records are kept and that’s okay. But data-driven epharma companies that don’t allow consumers to buy without prescriptions and keep a record of every transaction that anyone can audit have to face uncertainty in terms of policy and regulations.
Building A Culture Of Healthtech Innovation
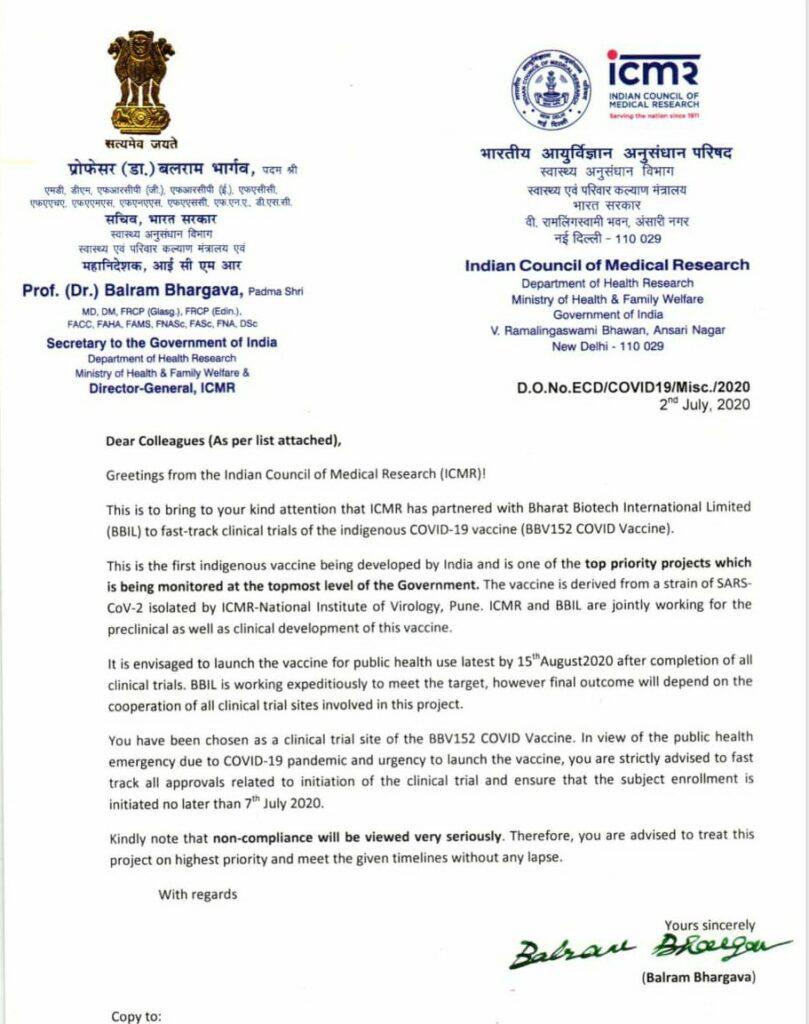
Forget policies, even the research & development, innovation works are now being heavily misguided and being mishandled by the government, a startup founder said on the condition of anonymity, indicating how ICMR is mishandling the entire Covid-19 vaccination trial.
There’s more to it. He said just because the PM wants to announce the launch of the world’s first vaccination from the Red Fort, the entire medical procedure is being overlooked. It is worth noting that the ICMR director general and secretary, dept of health research, ministry of health and family welfare Dr Balram Bhargava on July 2 had issued a letter directing Bharat Biotech, maker of Covaxin, a possible vaccine of Covid-19 to fast track the clinical trial and make it ready by August 15. Almost all the medical experts across the world are of the opinion that it would not only set a bad precedent but it is making a mockery of the entire clinical trial process.
Dr Jotwani said healthcare administration remains a major issue. People who are making decisions need to understand the gravity of seriousness healthcare requires? How pandemics happen or work or how a disease process works? How does it affect individuals? Those decisions should be managed or should be made by people who are experts in that area.
Founders also said that you can’t force startups to come up to innovate in healthcare. Startups will chase opportunities wherever there is clarity that their operations won’t be blocked by regulations, as has happened for online pharmacies.
Unlike the other sectors, one of the major challenges with the healthtech startups is the longer timeframe needed to conceptualize, create and validate the products or undertake clinical research in areas of medicine and vaccination. Startups need a support system to overcome these challenges. Portea’s Meena Ganesh said that the support system for such research and development initiatives is still in the nascent stages in India. There is a need to provide an incubator ecosystem for such companies wherein they are provided an opportunity to work in tandem with the government facilities and institutions such as ICMR.
Further, there are certain regulatory challenges that need to be overcome when it comes to development of drugs, vaccines and therapies in India. There is an urgent need to provide financial support in the form of funding and investments as well as tax benefits. By helping the innovators with their financial concerns and offering incentives to those who create transformational products and services in the healthcare sector, the government can ensure greater long-term improvement of the quality of life in the country. Alongside the support provided by healthcare incubators and institutional research facilities, this financial independence can boost healthtech and e-pharma companies tremendously,” Ganesh added.
Varun Gera, founder and CEO of HealthAssure, however believes that if one has to prioritise about the demands from the government to help boost healthtech infrastructure, funding may not be his top priority.
“The centre is even struggling to pay states their SGST stake. We are clearly not in a situation where we would expect something from the government in terms of funding support. Even if there would be some announcement it may be to the tune of INR 100-300 Cr. That won’t create much of the difference.”
However, what the government may ensure is that the enabling market it could create by removing regulatory and unnecessary tax hurdles, Gera asserted.
Startup-related innovations are mostly demand-driven which then oblige the government to come up with a suitable solution. Ankit Chaudhari, CEO & founder, Aiisma, a data marketplace app with symptom mapping feature opined that the DND feature facilitated by TRAI was indeed a user-driven feature. It was the demand and data privacy concerns raised by users which forced TRAI to come up with this feature.
Similar is the case with healthcare innovations in India — it has to be demand-driven, said Chaudhari.
Finding a balance between private and public healthcare, conventional and virtual healthcare, establishing a data-sharing architecture and ensuring data privacy won’t be an easy job. And, if policies are not ready for the changing healthcare ecosystem, things will only go south from wherever we are.























 Ad-lite browsing experience
Ad-lite browsing experience